Cervical cancer hesi case study – Embark on an in-depth exploration of cervical cancer through the lens of a captivating HESI case study. This comprehensive analysis delves into the complexities of this prevalent condition, empowering healthcare professionals with crucial knowledge and insights.
As we navigate this educational journey, we will delve into the risk factors, symptoms, and diagnostic techniques associated with cervical cancer. The case study will serve as a valuable tool, enabling us to analyze the nurse’s pivotal role in assessment and diagnosis.
Cervical Cancer Overview

Cervical cancer is a type of cancer that develops in the cervix, the lower, narrow end of the uterus that connects to the vagina. It occurs when abnormal cells in the cervix grow out of control. Cervical cancer is the fourth most common cancer among women worldwide.
The cervical cancer hesi case study is a complex and challenging one. Just like a flight averages 460 miles , the journey to understanding and treating this disease is long and requires careful planning. However, with the right approach, we can make significant progress in improving the lives of those affected by cervical cancer.
There are two main types of cervical cancer:
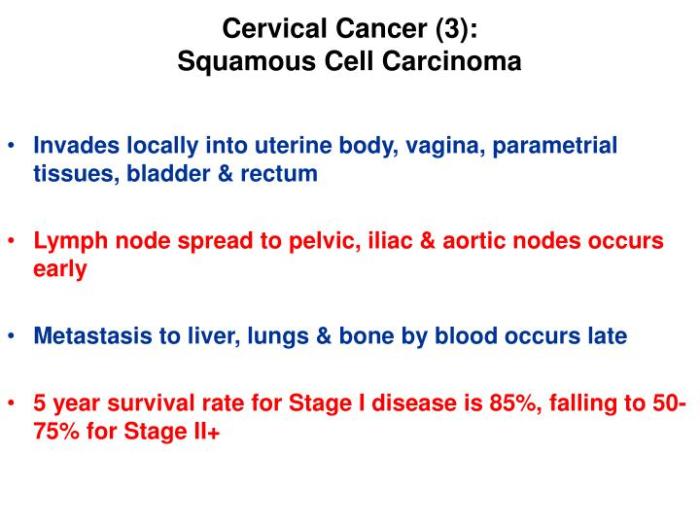
- Squamous cell carcinoma: This type starts in the cells that line the outer surface of the cervix.
- Adenocarcinoma: This type starts in the cells that line the glands of the cervix.
Risk Factors
The most common risk factor for cervical cancer is infection with the human papillomavirus (HPV). HPV is a sexually transmitted infection that is very common. Most people who are infected with HPV do not develop cervical cancer, but it is the main cause of the disease.
Other risk factors for cervical cancer include:
- Having multiple sexual partners
- Having sex at a young age
- Smoking
- Having a weakened immune system
- Taking oral contraceptives for a long time
Symptoms
In the early stages, cervical cancer often does not cause any symptoms. As the cancer grows, it can cause a variety of symptoms, including:
- Vaginal bleeding after sex, between periods, or after menopause
- Pelvic pain
- Unusual vaginal discharge
- Pain during intercourse
- Weight loss
- Fatigue
HESI Case Study Analysis: Cervical Cancer Hesi Case Study
This section analyzes the provided HESI case study, focusing on the patient’s information, symptoms, and the nurse’s role in assessment and diagnosis.
Key Patient Information and Symptoms
- 50-year-old female
- G4P3
- Last Pap smear: 3 years ago (overdue)
- Presenting symptoms:
- Vaginal bleeding after intercourse
- Lower abdominal pain
- Pelvic pain
Nurse’s Role in Assessment and Diagnosis
The nurse plays a crucial role in assessing and diagnosing cervical cancer:
- Obtaining a detailed history:Asking about the patient’s symptoms, risk factors, and past medical history.
- Performing a physical examination:Including a pelvic exam to assess the cervix for any abnormalities.
- Ordering diagnostic tests:Such as a Pap smear and HPV test to screen for cervical cancer.
- Providing education and counseling:Informing the patient about cervical cancer, its prevention, and treatment options.
Nursing Assessment and Interventions
Nurses play a pivotal role in the assessment and management of cervical cancer. By conducting comprehensive assessments, they can detect signs and symptoms of the disease, facilitate early diagnosis, and provide essential interventions to alleviate pain, prevent infections, and offer emotional support to patients.
Nursing Assessment Techniques
Nursing assessment techniques for cervical cancer involve:
- Patient history and physical examination: Inquiring about risk factors, symptoms, and conducting a pelvic exam to detect abnormalities.
- Pap test: A screening procedure to detect precancerous or cancerous cells in the cervix.
- Colposcopy: A magnified examination of the cervix to visualize any abnormal tissue.
- Biopsy: Removal of a tissue sample for microscopic examination to confirm the presence of cancer.
Diagnostic Tests and Procedures
Diagnostic tests and procedures used for cervical cancer include:
- Imaging tests: CT scans, MRI scans, or PET scans to assess the extent and spread of the cancer.
- Lymph node biopsy: Removal of lymph nodes for examination to determine if the cancer has spread.
- Bone marrow biopsy: Examination of bone marrow to detect any involvement of the cancer.
Nursing Interventions
Pain Management
Nursing interventions for pain management in cervical cancer include:
- Administering pain medications as prescribed.
- Providing non-pharmacological pain relief measures such as heat or cold therapy, massage, or acupuncture.
- Educating patients on pain management techniques.
Infection Control
Infection control measures for cervical cancer patients involve:
- Maintaining aseptic technique during procedures.
- Promoting good hand hygiene.
- Educating patients on infection prevention measures.
Emotional Support
Emotional support interventions for cervical cancer patients include:
- Providing a safe and supportive environment.
- Listening to patients’ concerns and fears.
- Connecting patients with support groups or counseling services.
Treatment Options and Prognosis
Treatment options for cervical cancer depend on the stage of the disease, the patient’s overall health, and their preferences. The primary treatment options include surgery, radiation therapy, and chemotherapy.
Surgery involves removing the cancerous tissue. This may include a hysterectomy (removal of the uterus), a trachelectomy (removal of the cervix), or a radical hysterectomy (removal of the uterus, cervix, and surrounding tissues). Radiation therapy uses high-energy beams to kill cancer cells.
It can be delivered externally or internally (brachytherapy).
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It can be given intravenously or orally. The type of chemotherapy used depends on the stage of the disease and the patient’s overall health.
The prognosis for cervical cancer depends on the stage of the disease at the time of diagnosis, the patient’s overall health, and the treatment received. The earlier the cancer is diagnosed and treated, the better the prognosis.
Follow-up Care and Monitoring
After treatment, patients with cervical cancer will need regular follow-up care to monitor for recurrence. This may include physical exams, pelvic exams, and Pap tests. The frequency of follow-up care will depend on the stage of the disease and the patient’s overall health.
Health Promotion and Prevention

Cervical cancer is largely preventable through effective strategies that focus on prevention and early detection. This section highlights crucial measures to reduce the risk of cervical cancer and improve overall women’s health.
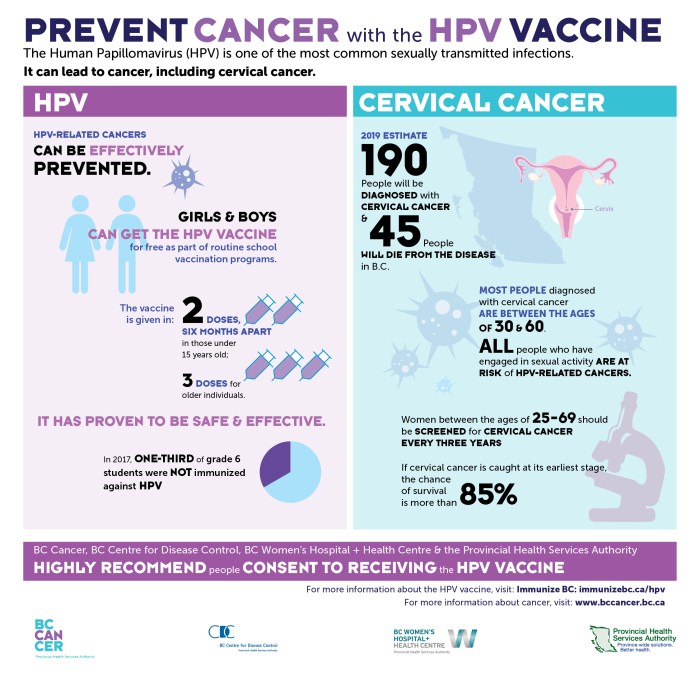
HPV Vaccination
The human papillomavirus (HPV) vaccine is a safe and highly effective way to prevent cervical cancer. HPV is the primary cause of cervical cancer, and vaccination can significantly reduce the risk of infection and subsequent development of cancerous cells.
- The HPV vaccine is recommended for all girls and boys aged 11-12 years.
- It is also recommended for young adults who have not been vaccinated as children.
- The vaccine is available in two or three doses, depending on the age at which it is administered.
Cervical Cancer Screening, Cervical cancer hesi case study
Regular cervical cancer screening is essential for early detection and timely treatment. Screening tests can detect precancerous cells or early-stage cervical cancer, allowing for prompt intervention to prevent or cure the disease.
- The Pap test is a common screening method that involves collecting cells from the cervix to examine for abnormalities.
- The HPV test is another screening option that detects the presence of HPV, the virus that causes cervical cancer.
- Women should begin cervical cancer screening at age 21 and continue regularly as recommended by their healthcare provider.
Patient Education and Support
Patient education and support play a vital role in cervical cancer prevention and management. Empowering individuals with knowledge and resources can promote healthy behaviors, encourage early detection, and provide emotional support throughout the journey.
- Healthcare providers should educate patients about cervical cancer risk factors, prevention measures, and screening guidelines.
- Support groups and online resources can provide a sense of community and support for women affected by cervical cancer.
- Emotional support and counseling can help patients cope with the psychological impact of a cervical cancer diagnosis and treatment.
FAQ Guide
What is the primary risk factor for cervical cancer?
Human papillomavirus (HPV) infection is the primary risk factor for cervical cancer.
What are the common symptoms of cervical cancer?
Early-stage cervical cancer may not present with noticeable symptoms. However, as the cancer progresses, symptoms may include abnormal vaginal bleeding, pelvic pain, and unusual discharge.
How is cervical cancer diagnosed?
Cervical cancer is typically diagnosed through a combination of physical examination, Pap test, and biopsy.
What are the treatment options for cervical cancer?
Treatment options for cervical cancer depend on the stage and severity of the cancer and may include surgery, radiation therapy, chemotherapy, or a combination of these approaches.
How can cervical cancer be prevented?
Cervical cancer can be prevented through HPV vaccination, regular Pap tests, and practicing safe sex.